Have you ever reached out to grab something, only to feel like your arm just isn’t cooperating? That strange feeling—where one or both arms feel weak, heavy, or hard to control—can be unsettling. Sometimes it’s nothing serious, but other times, it’s a warning sign from your body you shouldn’t ignore.
Let’s break it down together.
What Is Arm Weakness?
Arm weakness is when your muscles feel less strong than usual, making it difficult to lift, carry, or move your arms like you normally would. This might happen suddenly or develop gradually over time. You might notice:
- Trouble lifting even light objects
- Feeling like one arm is heavier than the other
- Tingling, numbness, or pain
- Your grip getting weaker
In some cases, it affects just one arm. In others, both arms feel weak. According to neurology clinics, arm weakness is a common reason people seek medical advice—especially when it happens suddenly.
How Does It Happen?
Your brain and spinal cord work together like a central command system. They send messages through nerves to tell your muscles when and how to move. Arm weakness usually happens when this system gets disrupted.
Here’s an easy analogy: imagine trying to water a garden, but the hose has a kink. Even though the water source is fine, the flow is blocked. Similarly, when nerves are pinched, injured, or diseased, the signal to your arm muscles becomes weak or lost altogether.
Depending on the location of the “kink”—whether it’s in your neck, shoulder, nerves, or brain—the type and severity of weakness can vary.
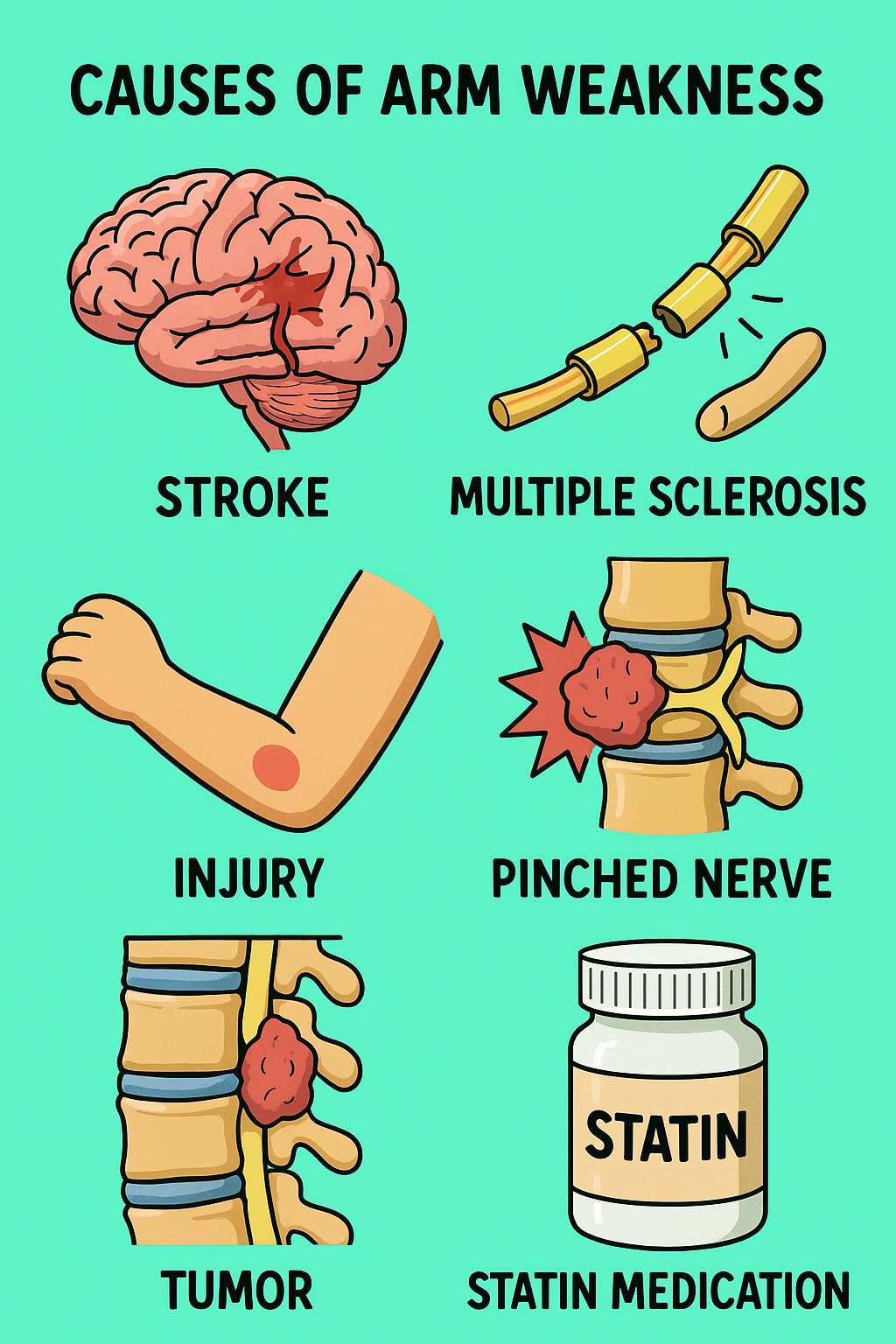
What Causes Arm Weakness?
Sometimes the cause is as simple as overuse or a pinched nerve. Other times, it’s linked to serious conditions like a stroke or nerve disease. Here’s a quick breakdown:
Common Causes:
- Pinched nerve in the neck or shoulder: (e.g., cervical radiculopathy from a slipped disc)
- Stroke: Sudden weakness on one side, often with facial droop or speech problems
- Neurological diseases: Such as multiple sclerosis (MS) or amyotrophic lateral sclerosis (ALS)
- Peripheral neuropathy: Often due to diabetes, alcoholism, or infections
- Muscle disorders: Like muscular dystrophy or myositis
- Injuries: Such as rotator cuff tears, fractures, or nerve trauma
- Autoimmune diseases: Like Guillain-Barré syndrome or myasthenia gravis
Risk Factors
So, who’s more likely to develop arm weakness? It depends on the cause, but here are some general risk factors:
- Age over 50 – higher risk of nerve compression and stroke
- Diabetes – increases nerve damage risk
- Smoking – worsens circulation and nerve health
- Sedentary lifestyle – weak muscles and stiff joints
- High blood pressure – raises stroke risk
- Previous injury – especially to the neck, shoulder, or arm
- Family history – of neurological or muscular disorders
Even simple things like poor posture or repetitive movements (e.g., typing, carrying heavy bags) can lead to nerve compression and weakness over time.
Other Symptoms That May Appear
Arm weakness doesn’t always come alone. Here’s what else to watch out for:
Common Associated Symptoms:
- Tingling or numbness
- Burning or sharp pain (especially from nerve-related causes)
- Muscle cramps or twitching
- Difficulty gripping or holding objects
Serious Warning Signs:
- Sudden onset of weakness, especially on one side
- Slurred speech or facial drooping
- Loss of coordination or balance
- Severe headache or vision changes
If you notice any of these red flags, go to the emergency department immediately—you could be having a stroke.
Tests to Identify the Cause
The key to treating arm weakness is understanding what’s causing it. Your doctor may start with:
- Physical and neurological exam – checking strength, reflexes, and sensation
- Blood tests – to detect infections, inflammation, or muscle enzymes
- Imaging (e.g., MRI, CT scan, or X-rays) – to look for stroke, pinched nerves, or injuries
- Nerve conduction studies (NCS) or EMG – to check how well your nerves and muscles communicate
- Lumbar puncture – if autoimmune or brain infection is suspected
Each test helps rule out different conditions until the source of the weakness is pinpointed.
Treatment for Arm Weakness
Treatment depends entirely on the cause. There’s no one-size-fits-all fix—but here’s a general idea:
Main Treatment:
- Stroke-related weakness:
- Emergency treatment (thrombolysis) within 3–4.5 hours of symptom onset
- Followed by rehabilitation: physical, speech, and occupational therapy
Other Treatments:
- Pinched nerve or herniated disc:
- Physical therapy, posture correction, anti-inflammatory medications
- Sometimes surgery if severe
- Muscle or joint injuries:
- Rest, ice, painkillers, physiotherapy
- Autoimmune or neurological disorders:
- Medications like steroids, immunosuppressants, or IV immunoglobulin
- Peripheral neuropathy:
- Managing diabetes, quitting alcohol, vitamin B12 supplements
- General muscle weakness:
- Strength training, occupational therapy, and treating the root illness
Sometimes, recovery takes weeks or even months—especially in stroke or autoimmune diseases. But many people regain full strength with the right help and consistency.
Final Thoughts
Arm weakness isn’t just about feeling a bit tired or sore—it can be your body’s way of waving a red flag. Some causes are minor and reversible. Others are serious and time-sensitive.
So if you’re thinking, “My arm feels weird today. Should I just wait it out?”—check in with a healthcare provider, especially if it’s sudden, getting worse, or affecting daily life.
References
- Arm Weakness – Symptoms and Causes, Cleveland Clinic (2023). https://my.clevelandclinic.org/health/symptoms/17607-arm-weakness
- Arm Weakness: Causes, Diagnosis, and Treatment, Healthline (2022). https://www.healthline.com/symptom/arm-weakness
- National Institute of Neurological Disorders and Stroke (NINDS). https://www.ninds.nih.gov/health-information/disorders
- Stroke Information, American Stroke Association (2023). https://www.stroke.org/en/about-stroke
