Ever looked down after using the toilet and noticed your stool is black? It can be a bit of a shock, especially if you weren’t expecting it. Black stool, also known as melena, is a symptom that often raises alarm bells. But what exactly does it mean?
In simple terms, black stool usually signals the presence of digested blood somewhere in your upper digestive tract — most often from the esophagus, stomach, or the first part of the small intestine. It’s less about what you ate and more about what might be happening inside your body. Did you know? About 1 in 400 adults who go to the hospital with gastrointestinal symptoms will have melena. It’s not super common, but it’s not exactly rare either.
Why Does Black Stool Happen?
Let’s break it down. Imagine your digestive system as a long, winding river. If there’s a bleed somewhere upstream (like the stomach), the blood travels through your gut, gets mixed and digested, and by the time it leaves your body, it turns black — like coffee grounds. That’s because stomach acids and enzymes break down the red blood cells and iron in the blood, changing their colour.
But not all black stools are created equal. Sometimes, what you eat or the medications you take can also be to blame. So, before you panic, think: did you recently have a lot of black licorice, blueberries, or iron supplements?
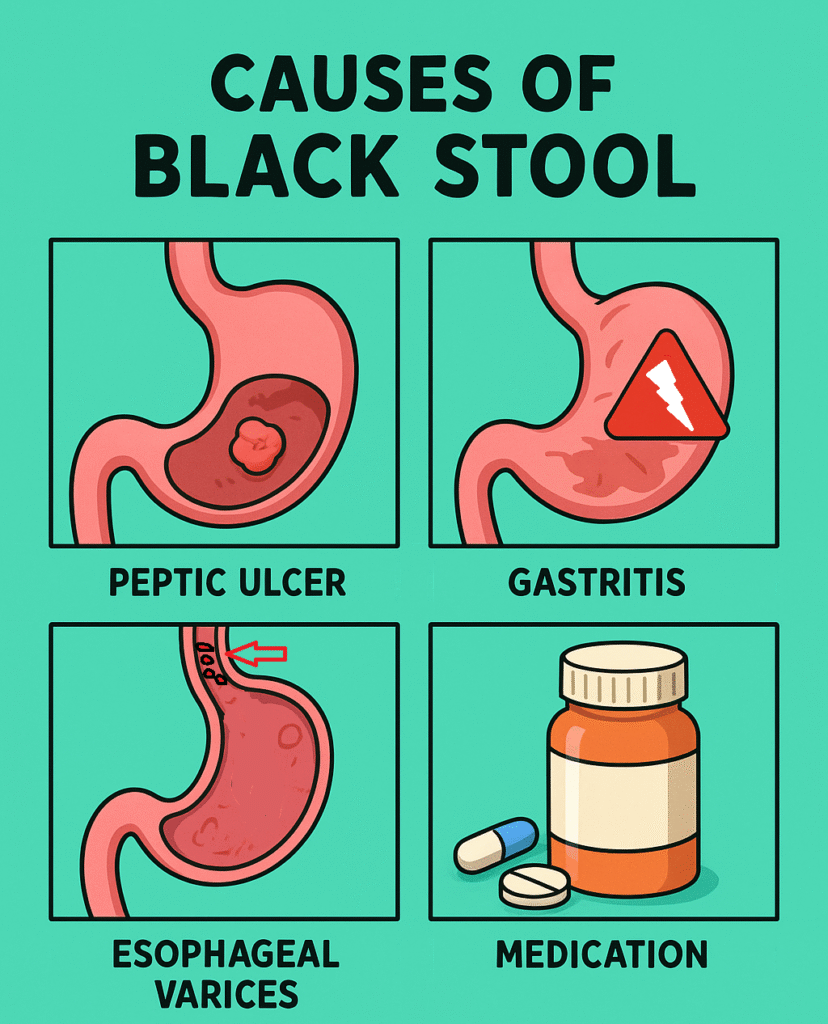
What Causes Black Stool?
Black stool can happen for several reasons. Some are serious, while others are harmless.
- Gastrointestinal bleeding:
This is the most concerning cause, responsible for the majority of cases. In about 70% of patients with black stool, bleeding from the upper digestive tract is the culprit.- Peptic ulcers (45%): Ulcers in the stomach or upper small intestine can bleed slowly, causing melena.
- Gastritis (inflammation of the stomach lining, 15%): Often due to alcohol, stress, or NSAID painkillers.
- Esophageal varices (10%): Swollen veins in the food pipe, usually related to liver disease.
- Mallory-Weiss tear (5%): Small tears in the esophagus, often from forceful vomiting.
- Stomach or esophageal cancer (3%): Less common, but important not to miss.
- Other causes (2%): Such as vascular malformations, or rare conditions.
- Medications and Foods:
Not all black stools are dangerous. About 20% of cases are caused by:- Iron supplements
- Bismuth-containing medications (like Pepto-Bismol)
- Foods like black licorice, blueberries, or even lots of dark chocolate
- Other less common causes:
- Bleeding disorders
- Swallowing blood (e.g., after a nosebleed)
Here’s a question to consider: Did you recently start a new medication or eat something unusual? Sometimes, the answer is right there.
Who Is Most at Risk?
Black stool can happen to anyone, but some people are more likely to develop it. Generally, adults over the age of 50, especially men, are at higher risk.
Top risk factors include:
- History of ulcers or gastritis
- Chronic use of NSAIDs or aspirin
- Heavy alcohol use
- Liver cirrhosis or liver disease
- Blood-thinning medications (like warfarin)
- Previous gastrointestinal bleeding
So, if you tick several of these boxes, it’s worth paying extra attention to any changes in your stool.
What Other Symptoms Should You Watch For?
Black stool rarely appears on its own. Often, there are other symptoms — some subtle, some impossible to ignore.
Common symptoms include:
- Stomach pain or discomfort
- Nausea or vomiting
- Weakness or fatigue
- Dizziness, especially when standing
When the disease gets more severe, you may notice:
- Vomiting blood (it may look like coffee grounds)
- Severe abdominal pain
- Fainting or feeling like you might pass out
- Pale, clammy skin
- Rapid heartbeat
If you ever see black stool with these severe symptoms, don’t wait — seek medical help immediately. Losing too much blood, even slowly, can be dangerous.
How Do Doctors Find the Cause?
The gold standard test to diagnose the source of black stool is called an upper endoscopy (or gastroscopy).
Here’s how it goes:
- You’ll usually be asked not to eat or drink for several hours before the procedure.
- You’ll receive a sedative to help you relax.
- A thin, flexible tube with a tiny camera at the end is gently passed through your mouth, down your esophagus, and into your stomach and upper intestine.
- The doctor can look for ulcers, bleeding, inflammation, or other abnormalities — and even treat some of them on the spot.
Expect to spend a few hours at the hospital or clinic, but most people go home the same day.
How Is Black Stool Treated?
Treatment depends on the cause. If the black stool is due to bleeding, doctors focus on stopping the bleed and preventing it from happening again.
- Mainstream Treatment (Gold Standard):
- Endoscopic therapy: During endoscopy, doctors can cauterise bleeding vessels, clip ulcers, or inject medications.
- Medications: Acid-suppressing drugs like proton pump inhibitors (PPIs) help heal ulcers and reduce further bleeding.
- If the first approach doesn’t work:
- Surgery: Rarely needed, but in severe or unmanageable cases, surgery may be required to remove the bleeding source.
- Transfusions: If there’s been a lot of blood loss, a blood transfusion may be needed.
- If food or medication is to blame:
Just stop the culprit and the black stool should resolve in a few days.
Above all, treatment isn’t one-size-fits-all. Your doctor will tailor the plan based on your specific cause and overall health.
References
- “Black or Tarry Stools: Causes and Treatments,” Healthline, 2023. https://www.healthline.com/health/black-stool
- “Melena: Causes, Diagnosis, and Treatment,” Cleveland Clinic, 2023. https://my.clevelandclinic.org/health/symptoms/21090-melena
- “Gastrointestinal Bleeding in Adults,” Mayo Clinic, 2022. https://www.mayoclinic.org/diseases-conditions/gastrointestinal-bleeding/symptoms-causes/syc-20372729
