Spotting blood in your stool can be alarming. It’s one of those things most people don’t want to talk about, but here’s the truth: it happens more often than you might think. Blood in the stool, also known as rectal bleeding, can be as subtle as a smear on toilet paper or as dramatic as a toilet bowl that suddenly looks like a horror movie. But don’t panic! Sometimes, the cause is harmless—but in other cases, it’s your body’s way of saying, “Hey, let’s get this checked.”
How common is it? Mild rectal bleeding affects up to 15% of adults each year . Most cases aren’t serious, but some do require medical attention. The key is knowing what’s normal, what’s not, and when to seek help.
How Does Blood Get Into Stool?
The digestive tract is like a long, winding tunnel. From your mouth all the way to your rectum, anything that disrupts the lining can cause bleeding. Imagine a garden hose: if it springs a leak anywhere along its length, water will drip out. In your gut, blood can leak from the upper parts (like the stomach) or lower parts (like the colon or rectum), and end up in your stool.
Bright red blood usually means the bleeding is from somewhere near the end of the digestive tract—like the rectum or anus. Dark, tarry stool (called melena) usually means the blood’s been digested, so the bleeding likely started higher up, such as in the stomach or small intestine.
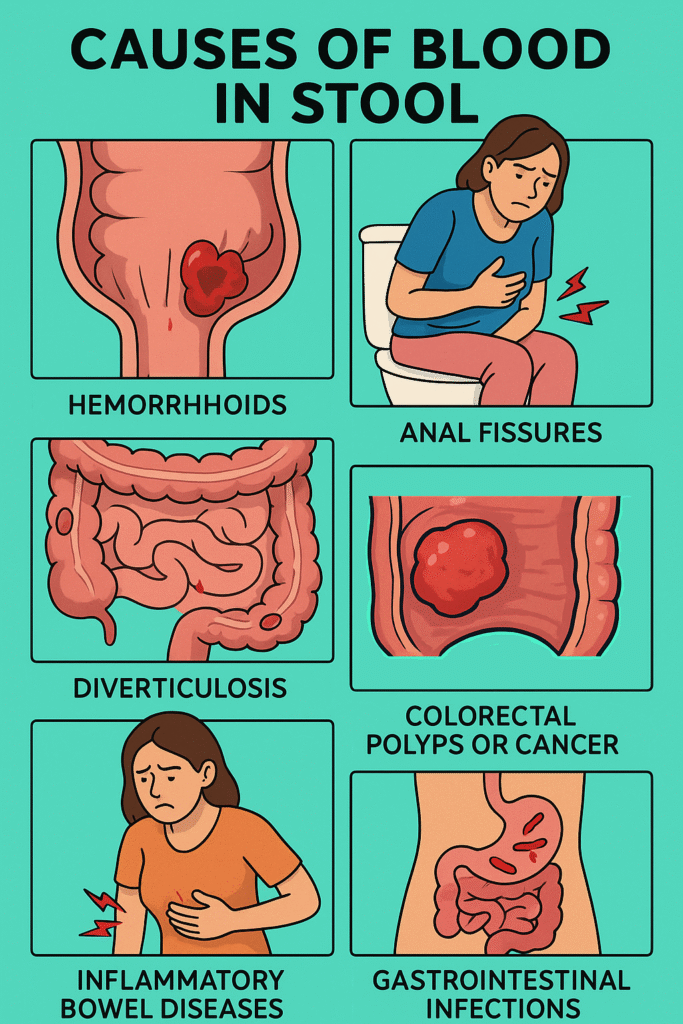
What Causes Blood in Stool?
Bleeding can happen for lots of reasons. Here’s a quick intro: most cases are caused by conditions like haemorrhoids or anal fissures—both uncomfortable but not life-threatening. More serious causes include infections, inflammatory bowel diseases, or even cancers.
Let’s break down the main culprits:
- Haemorrhoids (about 40–60% of cases): Swollen blood vessels around the anus or lower rectum. Common in adults, especially during pregnancy or after straining with constipation.
- Anal fissures (up to 15%): Small tears in the lining of the anus, often from passing hard stools.
- Diverticulosis (5–10%): Small pouches in the colon wall that can bleed.
- Colorectal polyps or cancer (less common, but important to rule out): Growths in the colon or rectum. Polyps are usually benign, but some can turn into cancer.
- Inflammatory bowel diseases (IBD), like Crohn’s or ulcerative colitis (about 5%): Cause inflammation and ulceration in the digestive tract.
- Gastrointestinal infections: Bacteria or viruses can inflame and damage the gut lining, leading to blood.
- Angiodysplasia: Fragile blood vessels in the colon, more common in older adults.
In rare cases, blood in stool can be linked to bleeding disorders or medication side effects (like blood thinners).
Risk Factors
Who’s most likely to notice blood in their stool? Honestly, it can happen to anyone, but certain groups are at higher risk.
- Adults over 50: Risk increases with age, especially for colorectal cancer and angiodysplasia.
- People with chronic constipation or who strain often: More likely to develop haemorrhoids or fissures.
- Those with a family history of colon polyps or colorectal cancer: Genetics play a role.
- Individuals with inflammatory bowel disease (IBD): Crohn’s or ulcerative colitis both boost the risk.
- People taking blood thinners or NSAIDs (like aspirin, ibuprofen): These medications make bleeding more likely.
- Pregnant women: Haemorrhoids are especially common during pregnancy due to increased pressure in pelvic veins.
A simple tip: if you fall into any of these categories, it’s extra important to pay attention to changes in your bowel habits.
Other Symptoms: What Else Should You Watch For?
Most people with blood in their stool notice only a streak of red on the toilet paper or in the bowl. But sometimes, other symptoms pop up:
Common symptoms:
- Itching, pain, or a lump near the anus (haemorrhoids or fissures).
- Abdominal cramps or pain.
- Changes in bowel habits (constipation, diarrhoea).
When things get more serious:
- Unexplained weight loss.
- Fatigue or weakness (a sign of chronic blood loss).
- Persistent changes in stool shape or frequency.
- Black, tarry stools (melena)—suggests upper GI bleeding.
- Large amounts of blood, dizziness, or fainting: this is a medical emergency.
Basically, if you see blood and feel unwell, or if bleeding continues, it’s time to call your doctor.
Tests to Identify the Cause
So, how do doctors figure out what’s going on? The gold standard test for blood in stool—especially if you’re over 40 or have other warning signs—is a colonoscopy.
What is a colonoscopy?
A colonoscopy is a procedure where a doctor uses a thin, flexible tube with a camera to look inside your colon and rectum. It’s usually done under mild sedation. The scope allows doctors to spot bleeding sources, take samples (biopsies), or even treat some problems right away (like removing polyps).
What to expect:
- You’ll need to empty your colon beforehand, usually with a special laxative (the “prep”).
- The test itself takes about 30–60 minutes.
- Most people can go home the same day.
- You might feel bloated or gassy afterward, but serious risks are rare.
Other tests, like stool tests (to check for hidden blood or infections), flexible sigmoidoscopy, or CT scans, might be used depending on your symptoms and age.
Treatment for Blood in Stool
The right treatment depends on what’s causing the bleeding.
Mainstream (Gold Standard) Treatment:
- Haemorrhoids: Lifestyle changes are first—more fibre, drinking plenty of water, and avoiding straining. Over-the-counter creams, warm baths, and, in some cases, minor procedures to shrink the haemorrhoids.
- Anal fissures: Similar advice—soften stools, use soothing ointments, and sitz baths.
- Diverticulosis: Bleeding usually stops on its own, but sometimes colonoscopy is needed to stop the bleed.
- Polyps or cancer: Removal during colonoscopy, surgery, or additional cancer treatments as needed.
- IBD: Medications to control inflammation (like steroids or immune-modifiers).
If first-line treatment doesn’t work:
- Procedures such as rubber band ligation for stubborn haemorrhoids.
- Surgical options for severe or persistent cases.
- Endoscopic techniques to stop bleeding or remove growths.
- Hospitalisation and blood transfusions in cases of heavy bleeding.
No matter the cause, early diagnosis and treatment usually lead to the best outcomes. Don’t ignore ongoing bleeding, even if it seems minor.
References
- Blood in Stool (Rectal Bleeding). Cleveland Clinic. Published 2023. https://my.clevelandclinic.org/health/symptoms/17781-blood-in-stool
- Rectal Bleeding: Causes, Symptoms, Diagnosis & Treatment. Mayo Clinic. Updated 2024. https://www.mayoclinic.org/symptoms/rectal-bleeding/basics/definition/sym-20050743
- Colonoscopy: What You Need to Know. NHS Inform. Reviewed 2022. https://www.nhsinform.scot/tests-and-treatments/procedures/colonoscopy
- Hemorrhoids and Anal Fissures. National Institute of Diabetes and Digestive and Kidney Diseases. Updated 2023. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids
- Rectal Bleeding: Should I Be Worried?. John Hopkins Medicine. Accessed 2024. https://www.hopkinsmedicine.org/health/conditions-and-diseases/rectal-bleeding-should-i-be-worried
