What is GERD?
Ever feel a burning sensation rising from your chest after a big meal? Or maybe you find yourself reaching for antacids a bit too often? That burning, uncomfortable feeling might not just be “bad food” — it could be GERD, short for Gastroesophageal Reflux Disease.
So, what is GERD, really? In the simplest terms, it’s a long-term condition where acid from your stomach repeatedly flows back up into your esophagus — the tube that carries food from your mouth to your stomach. This backwash, or “reflux,” irritates the lining of your esophagus and causes symptoms like heartburn.
You might be surprised to know GERD is incredibly common. In fact, about 20% of people in Western countries experience GERD symptoms regularly, according to several studies. That’s a lot of heartburn!
How Does GERD Happen? (The “Plumbing Problem” Analogy)
Let’s make it easy: imagine your stomach as a kitchen sink full of acidic “dishwater.” Between the sink and the drainpipe (your esophagus) is a valve — the lower esophageal sphincter (LES). Its job? Keep everything flowing in one direction: down.
But what if that valve is weak or leaky? Acid can splash back up the pipe, irritating the walls — just like dishwater spilling up your drain! Over time, repeated splashes cause damage, leading to the classic symptoms of GERD.
What Are the Causes of GERD?
Why does this “leak” happen? The truth is, GERD isn’t caused by just one thing. It’s more like a perfect storm of triggers. Here’s a quick overview (and some numbers for context):
- Weak LES muscle – This is the big one. If the valve at the end of your esophagus isn’t tight enough, acid slips back up. Roughly 70% of GERD cases involve a weak LES .
- Hiatal hernia – This is when a part of your stomach bulges up into your chest, making reflux more likely. It’s seen in about 50% of people with GERD.
- Obesity – Carrying extra weight puts pressure on your stomach, which can force acid upward.
- Pregnancy – Hormones and increased belly pressure make heartburn more common.
- Certain medications and foods – Things like NSAIDs, antihistamines, chocolate, caffeine, and spicy foods can relax the LES.
But sometimes, no obvious cause can be found — it just happens!
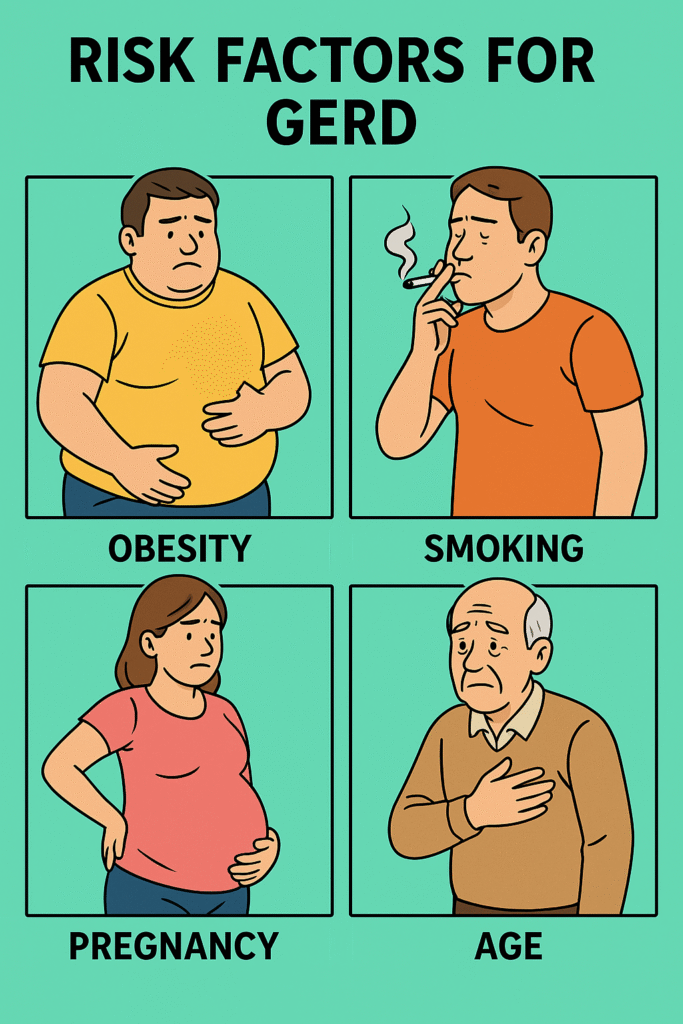
Who Is Most at Risk? (Risk Factors)
Do you ever wonder, “Am I at risk?” The truth is, GERD can affect anyone, but certain people have a higher chance. Before we dive into the list, here’s an important note: lifestyle choices play a big role!
Biggest risk factors:
- Obesity — Extra belly fat means more pressure on your stomach, increasing reflux risk .
- Smoking — Nicotine weakens that all-important LES valve.
- Pregnancy — As mentioned earlier, both hormones and pressure make reflux more likely.
- Age — GERD gets more common as we get older.
- Diet habits — Eating large meals, lying down after eating, or loving spicy/fatty foods? All can trigger reflux.
- Certain conditions — Hiatal hernia, delayed stomach emptying, or diabetes can increase your chances.
If you tick several of these boxes, your risk goes up. But even young, fit folks can develop GERD!
Symptoms of GERD: What Does It Feel Like?
So, what does GERD actually feel like? Heartburn is the classic symptom — a burning pain in the middle of your chest, especially after meals or at night. But GERD isn’t just about heartburn.
Common symptoms include:
- Heartburn (burning chest pain)
- Regurgitation (sour or bitter taste in your mouth)
- Difficulty swallowing (it can feel like food is stuck)
- Chronic cough or throat clearing
- Hoarseness or sore throat, especially in the morning
- Feeling like there’s a lump in your throat
Why do these happen? It’s all about the acid. When acid creeps up, it irritates the esophagus and even the throat, causing that burning, cough, or hoarse voice. Sometimes, GERD can masquerade as asthma or chronic cough — it’s a real chameleon.
What Else Could It Be? (Differential Diagnosis)
Here’s a tricky question: Is it always GERD? The reality is, several other conditions can look a lot like GERD. That’s why it’s important to see a doctor if symptoms persist.
Common “look-alikes”:
- Peptic ulcer disease – Causes burning stomach pain, especially if you’re hungry.
- Angina (heart pain) – Can mimic heartburn but is related to heart disease. Never ignore severe chest pain!
- Esophageal motility disorders – These affect how food moves down your esophagus.
- Gallbladder disease – Sometimes causes pain in the upper abdomen, especially after fatty meals.
- Infections (like candida or viruses) – Can cause painful swallowing.
Each of these can cause burning or discomfort in your chest or upper belly, just like GERD.
How Do Doctors Diagnose GERD?
Ever wonder how doctors are so sure it’s GERD? Usually, a classic story of heartburn and regurgitation is enough for a “working diagnosis.” But if symptoms are severe, unusual, or don’t improve, your doctor might order tests.
Gold standard test:
24-hour pH monitoring – This involves placing a tiny probe in your esophagus to measure acid levels over a day. If your esophagus is bathing in acid when it shouldn’t be, bingo — GERD confirmed.
Other tests may include:
- Endoscopy – A thin tube with a camera is passed down your throat to look for damage.
- Manometry – Checks how well your esophagus muscles work.
- Barium swallow – You drink a chalky liquid that shows up on X-ray.
But for most people, doctors start treatment based on symptoms alone.
Treatment: How Do You Get Rid of GERD?
Ready for some relief? Here’s the good news: Most cases of GERD can be managed with a mix of lifestyle tweaks and medication. Let’s break it down.
First up: Lifestyle changes (yes, really!):
- Lose weight if you’re overweight.
- Raise the head of your bed (try blocks or a wedge pillow).
- Eat smaller meals and avoid lying down after eating.
- Cut down on trigger foods — spicy, fatty, chocolate, coffee, and alcohol are the usual suspects.
- Stop smoking if you haven’t already.
Medications (Gold Standard):
- Proton pump inhibitors (PPIs) — like omeprazole, esomeprazole, rabeprazole, pantoprazole or lansoprazole. These block stomach acid and are the go-to meds for GERD .
- H2 blockers — like ranitidine or famotidine (less powerful but helpful for some).
- Antacids — for quick, temporary relief.
What if medicine doesn’t help?
For the small number of people who don’t get better with pills or can’t stop their meds, surgery is an option. The most common is called Nissen fundoplication, where the top of your stomach is wrapped around the lower esophagus to reinforce that leaky valve.
Other new, less invasive procedures exist, but they’re not as common.
Related Articles:
- Best Medications for GERD: PPIs, H2 Blockers & Antacids
- Home Remedies That Actually Help Relieve GERD
- When to Consider Surgery for GERD (Fundoplication & More)
- Can Intermittent Fasting Help with GERD?
- What Is Barrett’s Esophagus and How Is It Linked to GERD?
- Can GERD Cause Cough, Asthma or Sore Throat?
References
- Mayo Clinic. “GERD.” https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Definition & Facts for GER & GERD.” https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/definition-facts
- American College of Gastroenterology. “Diagnosis and Management of Gastroesophageal Reflux Disease.” https://gi.org/topics/gerd/
