Heel pain can sneak up on you. One day you’re walking just fine, and the next, each step feels like you’re stepping on a sharp stone. If that sounds familiar, you’re not alone—heel pain is one of the most common foot complaints, especially in adults. Let’s unpack what causes it, who’s at risk, and how to manage it effectively.
What is Heel Pain?
Heel pain refers to discomfort in the underside or back of the heel. It can be sharp or dull, constant or occasional, and sometimes it’s worse in the morning or after rest. The most common cause? Plantar fasciitis, which affects around 1 in 10 people during their lifetime.
Other causes include Achilles tendinitis, heel spurs, and nerve entrapment. Heel pain is especially common in people who are on their feet a lot, like runners, teachers, and retail workers.
How Does It Happen?
Your heel absorbs a lot of pressure—every step you take puts about 1.25 times your body weight on your feet. Over time, repetitive strain can damage the soft tissues in your heel, particularly the plantar fascia, a thick band that connects your heel bone to your toes.
Think of the plantar fascia like a bowstring under your foot. Too much tension or overuse causes microtears, inflammation, and pain. Similarly, the Achilles tendon, which connects the calf muscles to the heel, can become irritated with overuse or poor foot mechanics.
What Causes Heel Pain?
Heel pain isn’t caused by one thing alone. Here’s a quick breakdown of the most common causes:
- Plantar Fasciitis (Up to 80% of cases)
Microtears and inflammation of the plantar fascia from overuse, improper footwear, or flat feet. - Achilles Tendinitis
Inflammation of the Achilles tendon, often in runners or those with tight calf muscles. - Heel Spurs
Bony outgrowths from the heel bone. They don’t always hurt, but when they do, they can feel like a knife in your heel. - Bursitis
Inflammation of the fluid-filled sacs that cushion your heel. - Nerve Entrapment
Such as tarsal tunnel syndrome, where a nerve near the heel is compressed, causing tingling or burning. - Stress Fracture
Tiny cracks in the heel bone from repetitive impact, often in athletes.
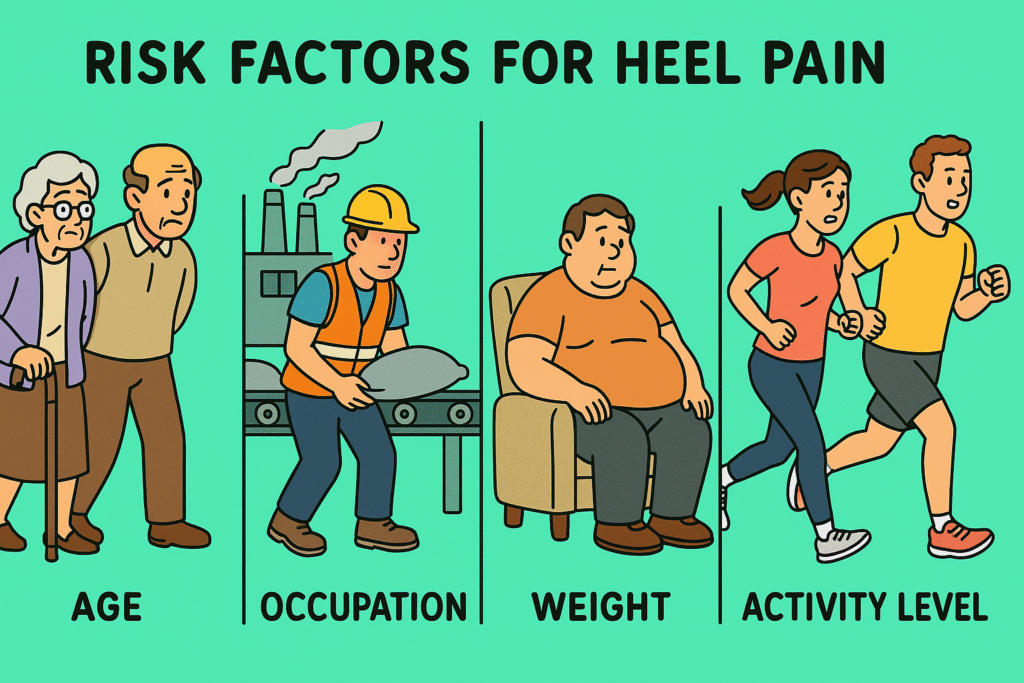
Risk Factors
Anyone can get heel pain, but some people are more likely to suffer from it. Here’s why:
- Age: Most common between ages 40–60
- Occupation: Jobs that involve standing or walking for long hours
- Footwear: Unsupportive shoes, especially with worn-out soles
- Foot Mechanics: Flat feet, high arches, or abnormal walking patterns
- Weight: Extra body weight adds more stress to the heel
- Activity Level: Runners, dancers, and athletes are at higher risk
- Health Conditions: Diabetes and arthritis can contribute to foot issues
Other Symptoms to Watch For
Heel pain is rarely just pain. It usually comes with other signs that can give clues to the cause:
- Morning pain: Common with plantar fasciitis. Pain often improves with movement.
- Stiffness or tight calf muscles: May signal Achilles tendinitis.
- Swelling or redness: Could be bursitis or infection.
- Numbness or tingling: May point to nerve involvement.
When heel pain becomes severe, you might start walking differently to avoid the discomfort. This can cause strain in your knees, hips, and back, creating a chain reaction of new problems.
Tests to Identify the Cause
The gold standard for diagnosing heel pain is a clinical examination by a doctor, but further tests may be needed:
- X-ray: Useful to spot heel spurs or rule out fractures
- Ultrasound: Great for visualising soft tissue problems like plantar fasciitis
- MRI: Reserved for complex cases to evaluate tendon or ligament damage
- Nerve conduction studies: If nerve compression is suspected
You’ll also be asked about your pain pattern, footwear, activity level, and medical history to build a full picture.
Treatment for Heel Pain
Most heel pain can be treated without surgery. The first goal is to reduce inflammation and give the tissues time to heal.
First-Line Treatments:
- Rest and activity modification: Avoid high-impact activities like running or jumping.
- Stretching exercises: Especially for the calf and plantar fascia
- Supportive footwear: Arch support and cushioned soles can make a big difference.
- Orthotic inserts: Custom or over-the-counter to correct abnormal foot mechanics
- Ice application: 15–20 minutes, several times a day
- NSAIDs (like ibuprofen): To reduce pain and swelling
- Night splints: To keep the foot in a stretched position overnight
If Pain Persists:
- Physical therapy: Helps improve strength and flexibility
- Corticosteroid injections: For short-term pain relief, though repeated use is discouraged
- Shockwave therapy: Uses sound waves to stimulate healing in chronic cases
- Surgery: Rare, but may be considered for severe, non-responsive plantar fasciitis
Final Thoughts
Heel pain may be common, but it shouldn’t be ignored. If your pain lasts more than a few weeks or starts interfering with your day-to-day life, it’s time to seek help. Early intervention can prevent chronic problems and keep you moving comfortably.
So, the next time your heels start complaining—listen. Your feet carry you through life. A little care can go a long way.
References
- Plantar Fasciitis – Diagnosis and Treatment. American Academy of Orthopaedic Surgeons (AAOS), 2023. https://orthoinfo.aaos.org/en/diseases–conditions/plantar-fasciitis
- Heel Pain Causes and Treatments. Mayo Clinic Staff, Mayo Clinic, 2022. https://www.mayoclinic.org/symptoms/heel-pain/basics/causes/sym-20050788
- Achilles Tendinitis – Patient Information. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), 2023. https://www.niams.nih.gov/health-topics/achilles-tendinitis
- Diagnosis and Management of Plantar Fasciitis. American Family Physician, 2021. https://www.aafp.org/pubs/afp/issues/2021/0201/p176.html
