What is Leg Weakness?
Leg weakness is a common symptom that makes your legs feel heavy, shaky, or lacking in strength. Some people describe it as their legs “giving way” or being unable to carry their body weight. It can happen suddenly or develop slowly over time.
While mild weakness can result from fatigue or lack of exercise, persistent or sudden leg weakness could point to a more serious medical condition involving the nerves, muscles, or even the brain.
How Does It Happen?
Let’s simplify how leg strength works: your brain sends signals down the spinal cord and through nerves to your leg muscles. If anything blocks or distorts these messages—like nerve damage, brain issues, or spinal problems—you may lose strength.
Imagine a power line delivering electricity from a station to your house. If there’s a break along the line (such as a fallen tree or damaged wire), your home won’t get the power it needs. Similarly, when the “communication line” from your brain to your leg muscles is disrupted, your legs may feel weak, numb, or useless.
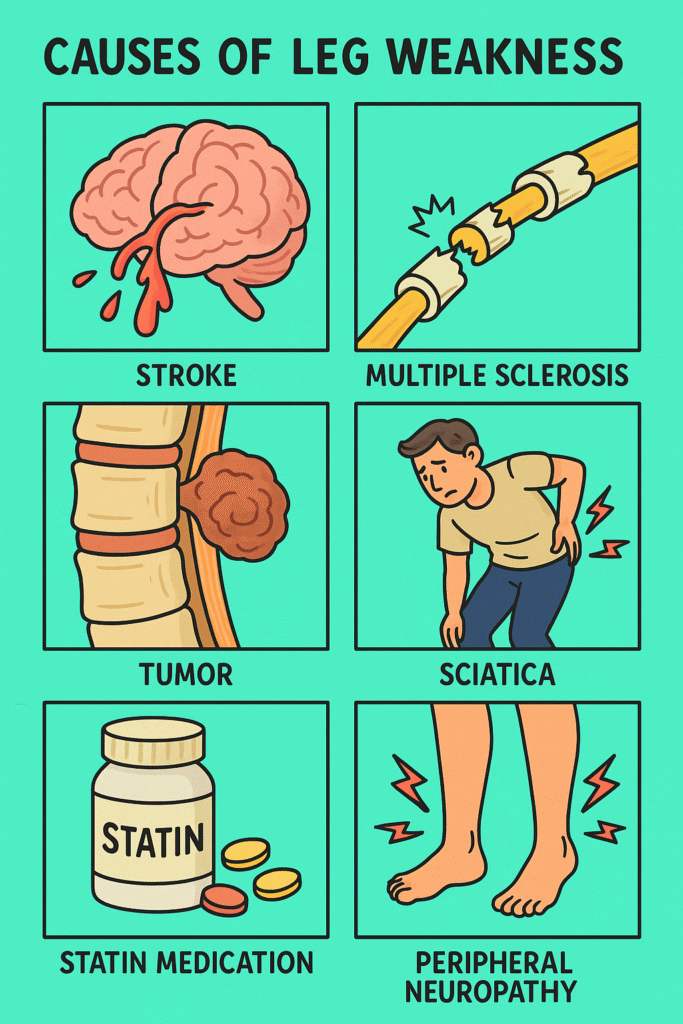
What Causes Leg Weakness?
Leg weakness can stem from many conditions. Here’s a breakdown of some common causes:
- Nerve-related conditions (Neurological causes)
These account for a large number of cases:- Stroke – sudden leg weakness, usually on one side
- Multiple sclerosis (MS) – progressive and may come and go
- Peripheral neuropathy – often caused by diabetes
- Pinched nerve or herniated disc in the lower back (sciatica)
- Muscle diseases (Myopathies)
These conditions affect the muscle fibers directly:- Muscular dystrophy
- Polymyositis or dermatomyositis
- Statin-induced myopathy (due to cholesterol-lowering drugs)
- Autoimmune or inflammatory conditions
- Guillain-Barré Syndrome – a rapid-onset muscle weakness due to nerve inflammation
- Lupus
- Metabolic and nutritional issues
- Low potassium or calcium
- Vitamin D or B12 deficiency
- Other causes:
- Infections (e.g., Lyme disease, HIV, or spinal infections)
- Tumours pressing on nerves or spinal cord
- Functional weakness (part of some psychological disorders)
Who is Most at Risk?
Anyone can experience leg weakness, but some people are more prone to it than others.
- Older adults: Especially those with chronic illnesses or muscle loss (sarcopenia)
- People with diabetes: Due to nerve damage (neuropathy)
- Sedentary individuals: Weak muscles from inactivity
- Those with autoimmune or neurological disorders: MS, lupus, or a family history
What Other Symptoms Might Come With It?
Leg weakness rarely comes alone. It may be accompanied by:
- Numbness or tingling
- Pain in the lower back or legs
- Muscle cramps
- Difficulty walking, standing, or climbing stairs
- Loss of balance
- Fatigue
- Bowel or bladder changes (a red flag symptom!)
If weakness suddenly appears or worsens, especially with signs like slurred speech, vision changes, or confusion, it may be a stroke—seek emergency care immediately.
Tests to Identify the Cause
The best diagnostic approach depends on the suspected cause. But in general, doctors may start with:
- Neurological exam – checking strength, reflexes, balance, and sensation
- Blood tests – to check electrolytes, inflammation, vitamins, and muscle enzymes
- MRI or CT scans – especially of the brain and spine
- Nerve conduction studies or EMG – to test nerve and muscle activity
- Lumbar puncture – to check for infections or autoimmune signs in spinal fluid
The gold standard test depends on the context. For example, in sudden one-sided weakness, a CT scan of the brain is the gold standard to check for stroke.
Treatment for Leg Weakness
Treatment depends on the underlying cause—but here’s the general plan:
1. Treat the root cause
- Stroke: Immediate clot-lytic drugs.
- Pinched nerve: Physical therapy, anti-inflammatory meds, or surgery.
- Low potassium: Electrolyte replacement.
- Myopathy: Adjust medications (like stopping statins), treat inflammation.
2. Supportive therapies
- Physical therapy to build strength, improve walking, and prevent falls
- Occupational therapy to help with daily activities
- Mobility aids like walkers or braces if necessary
3. Medications
- Anti-inflammatories
- Muscle relaxants
- Steroids or immunosuppressants (for autoimmune diseases)
- Pain medications (if nerve pain is present)
If the cause is not physical but psychological (known as functional neurological disorder), therapy and rehabilitation are crucial—and recovery is possible with the right support.
Final Thoughts
Leg weakness is a symptom—not a diagnosis. It’s like a warning light in your car—it could mean something minor, or it could signal a serious problem under the hood. Whether it creeps up slowly or hits you all at once, don’t ignore it. Identifying the root cause early can make all the difference in recovery and quality of life.
References
- Leg Weakness – Symptoms and Causes. Cleveland Clinic, April 25, 2023. https://my.clevelandclinic.org/health/symptoms/17620-leg-weakness
- Neurological Causes of Leg Weakness. National Institute of Neurological Disorders and Stroke (NINDS). https://www.ninds.nih.gov/
- Muscle Weakness Causes and Diagnosis. Mayo Clinic, May 2023. https://www.mayoclinic.org/symptoms/muscle-weakness
