Lower back pain is something many of us will experience at some point in life — maybe after lifting a heavy box, sitting for too long, or even just waking up one morning with an ache that wasn’t there the day before. But what exactly is lower back pain, and why does it affect so many people?
What is Lower Back Pain?
In simple terms, lower back pain refers to discomfort or aches localized in the area between the bottom of your rib cage and the top of your legs. This region supports much of your body weight and allows you to move, twist, bend, and stand upright.
It’s surprisingly common — studies suggest that nearly 80% of adults experience lower back pain at some point in their lives. For many, it’s temporary, lasting just a few days or weeks, but for others, it can become a chronic issue that affects daily life and mobility.
Have you ever wondered why a simple strain can linger for weeks? That’s where understanding how the lower back works can help.
How Does Lower Back Pain Happen?
Think of your lower back like the foundation of a tall building. It needs to be strong and flexible to support the structure above — your upper body — and handle everyday stresses. Your lower back consists of:
- Bones (vertebrae)
- Discs that cushion the bones
- Muscles and ligaments that support movement and stability
- Nerves that send signals to and from your brain
If any of these parts get injured, overused, or irritated, you feel pain.
Imagine your discs as small jelly-filled cushions between building blocks. If one gets squashed or herniated (meaning the jelly leaks out), it can press on nearby nerves, causing sharp, shooting pain down your leg (known as sciatica).
Or picture your muscles like rubber bands — if stretched too far or strained, they get tight and sore, making it painful to move.
What Causes Lower Back Pain?
Lower back pain can come from many sources. Sometimes it’s a sudden injury, like lifting something heavy the wrong way. Other times, it’s a slow build-up of stress from poor posture or repetitive movements.
Here are some of the main causes:
- Muscle or ligament strain: This is the most common cause. For example, lifting heavy objects without proper technique can strain muscles and ligaments.
- Bulging or herniated discs: When the cushioning discs between vertebrae bulge or rupture, they can irritate nerves.
- Arthritis: Osteoarthritis can affect the joints in your lower back, leading to pain and stiffness.
- Skeletal irregularities: Conditions like scoliosis (a sideways curve of the spine) can cause discomfort.
- Osteoporosis: Weak, brittle bones can lead to fractures, even from minor falls or stresses.
- Other causes: Infections, tumors, or inflammatory diseases (like ankylosing spondylitis) are less common but serious reasons.
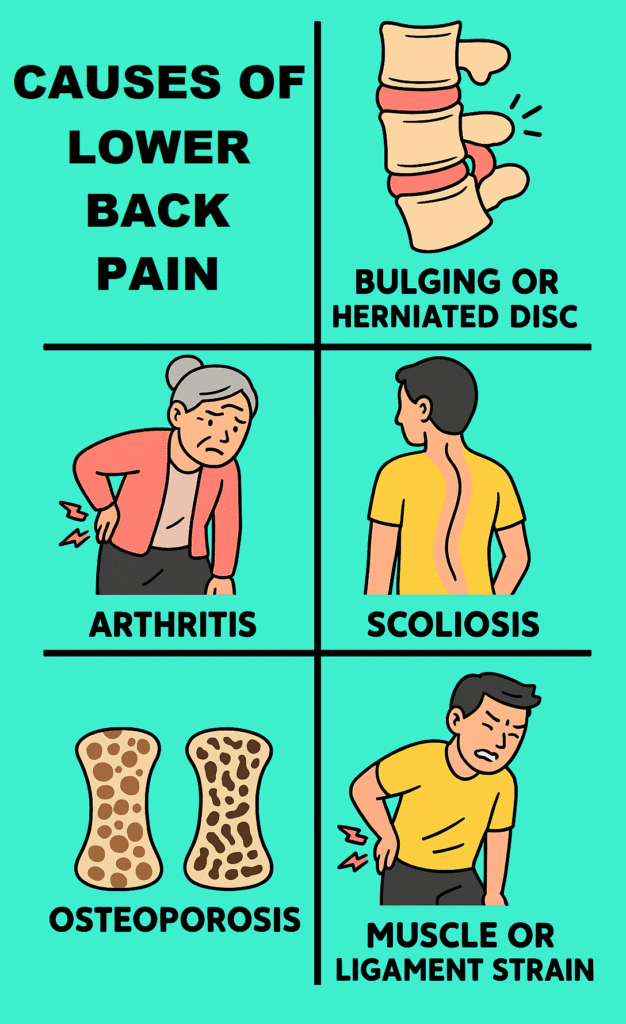
About 90% of lower back pain cases are due to muscle or ligament strain or disc problems.
Who is at Risk?
Anyone can get lower back pain, but some people are more likely to experience it. Here’s who tends to be at higher risk:
- People with sedentary jobs or lifestyles, especially those sitting for long periods.
- Those who do heavy physical work, especially without proper body mechanics.
- People who are overweight, putting extra stress on the back.
- Older adults — as we age, the spine’s discs and joints wear down.
- Individuals with poor posture habits.
- Smokers — smoking reduces blood flow to the spine, slowing healing.
- People with stress or depression, as pain perception can be heightened.
What Are the Symptoms?
Lower back pain isn’t just about feeling sore. It can vary widely:
- A dull, constant ache
- Sharp or stabbing pain when moving
- Stiffness and reduced range of motion
- Muscle spasms or tightness
- Pain radiating down the leg (sciatica)
When pain worsens or is accompanied by numbness, weakness, or loss of bladder or bowel control, it could signal a more serious problem needing urgent medical attention.
How Is Lower Back Pain Diagnosed?
Usually, doctors start with a physical exam and history — asking about the pain’s location, duration, and triggers. In many cases, imaging like X-rays, MRIs, or CT scans aren’t necessary unless symptoms persist or worsen.
The gold standard test when nerve involvement is suspected is an MRI, which shows soft tissues like discs and nerves clearly.
If you have severe or unexplained symptoms, your doctor might recommend blood tests or other scans to rule out infections or tumors.
Treating Lower Back Pain
The good news? Most lower back pain improves within a few weeks with simple measures. Here’s the usual approach:
- Rest and activity modification: Avoid heavy lifting or sudden movements but try not to stay in bed too long.
- Pain relief: Over-the-counter painkillers like ibuprofen or acetaminophen can help.
- Physical therapy: Guided exercises improve flexibility and strengthen muscles supporting the back.
- Heat or cold therapy: Ice packs reduce inflammation; heat relaxes tight muscles.
- Lifestyle changes: Improving posture, losing excess weight, quitting smoking, and regular low-impact exercise can prevent recurrence.
If pain persists beyond 6 weeks or is severe, other options include:
- Prescription medications (muscle relaxants, stronger painkillers)
- Injections (like corticosteroids)
- Surgery (rarely, but sometimes necessary for severe nerve compression)
Have you ever tried specific exercises or treatments for your back pain? Sometimes, small changes can make a big difference.
References
- Lower Back Pain Overview, Mayo Clinic, 2024. https://www.mayoclinic.org/diseases-conditions/back-pain/symptoms-causes/syc-20369906
- Low Back Pain Fact Sheet, National Institute of Neurological Disorders and Stroke, 2023. https://www.ninds.nih.gov/health-information/disorders/low-back-pain
- Guidelines for Management of Acute and Chronic Low Back Pain, American College of Physicians, 2021. https://www.acponline.org/clinical-information/guidelines
