Mouth ulcers—also known as canker sores—are small, painful sores that appear inside the mouth. They’re incredibly common and, while usually harmless, can be frustrating and uncomfortable. Whether it’s a sting when you sip orange juice or pain when brushing your teeth, mouth ulcers can interfere with your daily routine.
So, what exactly causes them? Are they a sign of something more serious? And what can you do to make them go away faster?
What Is a Mouth Ulcer?
A mouth ulcer is an open sore that forms on the soft tissues inside your mouth, including the inner cheeks, lips, tongue, or the floor of the mouth. These ulcers are typically round or oval, white or yellow in the centre with a red border. Unlike cold sores, which form outside the mouth and are caused by a virus, canker sores are non-contagious and happen inside the mouth.
Mouth ulcers are very common—up to 20% of the population experiences them at some point, and they tend to affect more females than males. They often first appear during adolescence or early adulthood.
How Do They Happen?
The process starts when the delicate lining of the mouth breaks or becomes inflamed. Think of your mouth’s inner lining as a protective cushion. When something irritates or damages that layer, it triggers an immune response, causing a sore to form.
Imagine accidentally biting your cheek. That tiny injury may seem insignificant, but it can spark a full-blown ulcer as your body tries to repair the damage. Sometimes, the immune system goes a bit overboard, and the area becomes inflamed and painful. That’s your classic canker sore.
What Causes Mouth Ulcers?
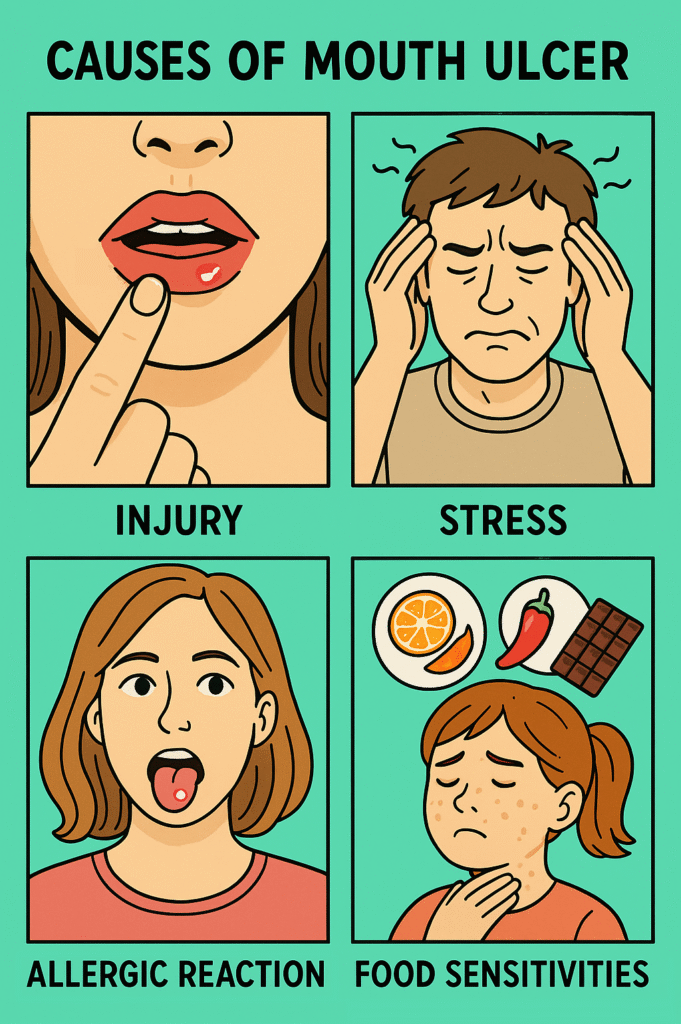
There are many possible causes, and sometimes more than one factor is involved.
Here are some of the common causes:
- Injury or trauma (e.g., biting your cheek, hard toothbrush, dental braces)
- Stress or fatigue
- Nutritional deficiencies, particularly of iron, folate (vitamin B9), and vitamin B12
- Hormonal changes, such as during menstruation
- Food sensitivities (e.g., citrus, spicy foods, or chocolate)
- Allergic reactions to toothpaste or mouthwash ingredients like sodium lauryl sulfate (SLS)
- Infections, such as viral infections (herpes simplex, hand-foot-and-mouth disease)
- Autoimmune diseases, including Behçet’s disease or lupus
- Gastrointestinal conditions, such as Crohn’s disease or celiac disease
Interestingly, around 40% of people with recurring ulcers have a family history of the same issue—suggesting genetics plays a role too.
Who’s at Risk?
Anyone can get a mouth ulcer, but some people are more likely than others.
You might be at greater risk if you:
- Are female (due to hormonal shifts)
- Have a family history of ulcers
- Have autoimmune or gastrointestinal disorders
- Frequently feel stressed or exhausted
- Have a weakened immune system
- Eat a nutrient-poor diet
Children and teens often get them more than older adults.
Other Symptoms
Most mouth ulcers are small and heal on their own within 7 to 14 days. But while they’re healing, they can be surprisingly painful—especially when eating, drinking, or talking.
Common symptoms include:
- A round or oval sore with a white or yellow centre and red edge
- Tingling or burning sensation before the ulcer appears
- Pain when eating spicy, salty, or acidic foods
- Mild swelling around the ulcer
Severe or more serious ulcers may include:
- Ulcers that last more than 3 weeks
- Larger or unusually shaped ulcers
- Multiple ulcers appearing at once
- Pain that spreads to the jaw or neck
- Fever, swollen lymph nodes, or fatigue
These may suggest a deeper problem and warrant a visit to the doctor.
Tests to Identify the Cause
For occasional mouth ulcers, no test is usually needed. A doctor or dentist can often diagnose them based on a simple visual exam.
But if ulcers are:
- Recurrent
- Severe
- Not healing
- Accompanied by other symptoms
…then tests may be needed. These can include:
- Blood tests to check for vitamin deficiencies or autoimmune diseases
- Swabs to rule out infections (e.g., herpes simplex)
- Biopsy (rare, but done if cancer or other serious condition is suspected)
The goal is to figure out whether the ulcers are a symptom of something deeper.
Treatment for Mouth Ulcers
Most ulcers heal without treatment. But there are ways to ease discomfort and speed up recovery.
First-Line Treatments (Gold Standard):
- Topical corticosteroids, like triamcinolone acetonide paste
- These reduce inflammation and help the ulcer heal faster
- Apply directly to the sore, usually 2–3 times daily
Other Options:
- Saltwater rinses – soothe pain and help prevent infection
- Over-the-counter gels – like benzocaine or lidocaine (numbing effect)
- Mouthwashes – especially those with chlorhexidine or antiseptic properties
- Nutritional supplements – if tests reveal a deficiency
- Avoiding triggers – such as spicy foods, acidic drinks, or certain toothpastes
If ulcers are caused by a medical condition (e.g., celiac disease or lupus), treating the underlying condition usually helps reduce outbreaks.
When to See a Doctor
Seek medical advice if:
- An ulcer doesn’t heal after 2–3 weeks
- You get them very frequently
- They’re unusually large or painful
- You experience fever, rashes, or other body symptoms along with them
Sometimes, what looks like a simple ulcer can actually be a sign of oral cancer—especially in older adults or smokers. It’s rare, but persistent sores should always be checked.
Final Thoughts
Mouth ulcers may be small, but they can pack a punch when it comes to pain and inconvenience. The good news is, most clear up quickly and aren’t dangerous. Still, if they keep coming back or seem unusually stubborn, don’t ignore them. Your body might be trying to tell you something important.
Curious if your diet or stress levels could be to blame? It’s worth tracking your flare-ups. Sometimes a small change—like switching toothpaste or getting more iron—can make a big difference.
References
- “Mouth Ulcers” – NHS (UK National Health Service), reviewed 2023. https://www.nhs.uk/conditions/mouth-ulcers/
- “Recurrent Aphthous Stomatitis” – American Family Physician, AAFP, 2020. https://www.aafp.org/pubs/afp/issues/2020/1001/p425.html
- “Canker Sores (Aphthous Ulcers)” – Mayo Clinic, reviewed 2024. https://www.mayoclinic.org/diseases-conditions/canker-sore/
