We’ve all had times when something just doesn’t feel right “down there.” One of the most uncomfortable? Pain while urinating. It can catch you off guard—maybe it’s a burning sensation, a sharp pain, or even just a weird discomfort. Whatever form it takes, it’s your body’s way of waving a red flag.
But what does it really mean when peeing hurts? Let’s break it down, from why it happens to how to deal with it—because nobody wants to keep dreading their next trip to the bathroom.
What is Pain During Urination?
Pain during urination (medical term: dysuria) is exactly what it sounds like: any pain, burning, or discomfort when you pee. It’s surprisingly common. In fact, millions of people see a doctor for this problem every year, with women being affected more often than men—mostly due to differences in anatomy.
Some quick facts:
- Up to 50% of women will experience at least one urinary tract infection (UTI) in their lives, with dysuria as a classic symptom.
- Men get it too, especially as they get older.
So, you’re definitely not alone if you’ve felt this before.
How Does Pain During Urination Happen?
Think of your urinary tract like a clean, well-maintained water pipe. Normally, pee flows through painlessly. But if something irritates the lining—like an infection or an injury—it’s like having a scratch inside the pipe. Suddenly, every drop stings as it passes by.
Here’s another way to picture it: imagine you have a tiny paper cut on your finger, and then you squeeze lemon juice on it. Ouch, right? That’s basically what happens when inflamed or damaged tissues in your urinary tract come in contact with urine.
The pain can be:
- At the start of urination (often points to a problem in the urethra).
- At the end or throughout (could mean the bladder is involved).
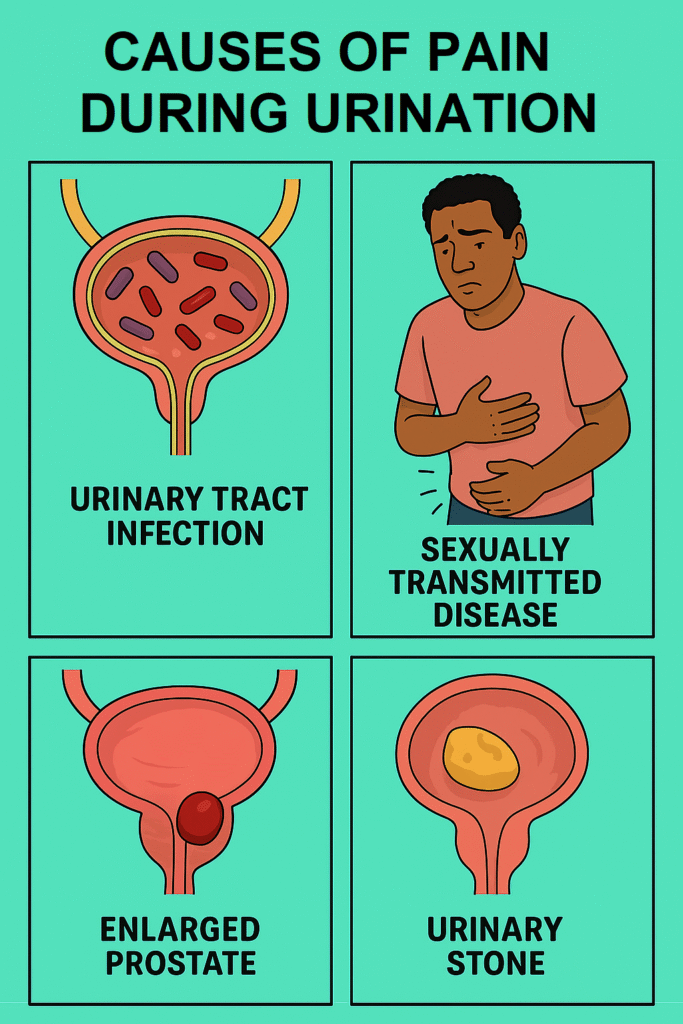
What Causes Pain During Urination?
When it comes to causes, there’s a shortlist of usual suspects, but the specifics can vary a lot. Sometimes it’s a simple infection. Other times, it’s something more.
Pain during urination can result from several things—most often an infection, but not always. It can be due to irritation, injury, or even certain medications. Knowing the cause is key to choosing the right treatment.
Let’s look at the main reasons:
1. Urinary Tract Infections (UTIs)
- By far the most common cause, especially in women (about 70–90% of cases).
- Bacteria (usually E. coli) enter the urinary tract, causing inflammation and pain.
2. Sexually Transmitted Infections (STIs)
- Chlamydia, gonorrhoea, herpes, and trichomoniasis can all cause dysuria.
- More common in sexually active young adults.
3. Bladder or Kidney Infections
- When a UTI travels upwards, it can involve the bladder (cystitis) or kidneys (pyelonephritis), leading to more severe pain and sometimes fever.
4. Prostatitis (in men)
- Inflammation of the prostate gland, common in men over 50, can make urination painful and difficult.
5. Vaginal or Urethral Irritation
- Non-infectious causes: scented soaps, bubble baths, douches, tight clothing, or even friction during sex.
- Allergic reactions or physical injury can inflame the area.
6. Urinary Stones
- Stones in the bladder or urethra can scrape the lining, causing sharp, stabbing pain.
7. Medications and Cancer Treatments
- Some drugs, especially chemotherapy, can inflame the bladder lining.
Risk Factors
Wondering if you’re more likely to experience this problem? Here’s a quick look at who’s most at risk.
Anyone can get dysuria, but some people are more likely to develop it based on their lifestyle, health, and anatomy.
Top Risk Factors:
- Being Female: Shorter urethra means bacteria have an easier path.
- Sexual Activity: Especially with new or multiple partners.
- Menopause: Reduced oestrogen can thin the urinary tract lining.
- Prostate Enlargement: Common in older men.
- Poor Hygiene: Not wiping front to back, holding in urine, etc.
- History of UTIs or Kidney Stones
- Use of Irritating Products: Scented soaps, spermicides.
- Chronic Medical Conditions: Diabetes weakens immunity and can increase risk.
So, if you tick any of these boxes, you might be at higher risk.
Other Symptoms: What Else Shows Up?
Pain during urination rarely comes alone. Usually, there’s an entourage of symptoms tagging along.
Depending on the cause, you may notice more than just pain when peeing. These extra clues help doctors zero in on what’s really going on.
Common Symptoms:
- Frequent Urges: Feeling like you have to go all the time, even if little comes out.
- Urgency: Sudden, strong need to pee.
- Cloudy, Bloody, or Foul-Smelling Urine
- Lower Belly or Back Pain
- Fever or Chills: May signal a spreading infection.
- Discharge: From penis or vagina (points to STIs).
- Itching or Irritation: Around the genital area.
Severe Signs:
- High fever
- Vomiting
- Severe back pain
- Inability to pee
If these happen, seek medical help immediately. They can be signs of kidney infection or blockage.
Tests to Identify the Cause
How do doctors figure out what’s going on? There’s a gold standard, plus a few other tools.
Urine Analysis and Culture
- What is it?
You’ll be asked to provide a clean-catch urine sample. Basically, pee in a cup after cleaning yourself, so outside bacteria don’t contaminate the sample. - What does it show?
- Looks for white blood cells (infection), red blood cells (bleeding), bacteria, or other problems.
- If infection is suspected, the urine is “cultured”—grown in a lab to see what bacteria are present and which antibiotics will work best.
- What to expect:
It’s quick, painless (except for the peeing part), and results usually come back in a day or two.
Other possible tests:
- STI screening: Swabs or urine tests if a sexually transmitted infection is suspected.
- Ultrasound or CT scan: If stones or blockage are possible.
- Cystoscopy: Rare, for complicated cases—using a tiny camera to look inside your bladder.
Treatment for Pain During Urination
Treatment depends on what’s causing your symptoms. Thankfully, most cases are treatable, and relief is often quick.
Mainstream (Gold Standard) Treatments
- UTIs:
Short course of antibiotics, usually 3–7 days. Symptoms often improve within 48 hours. - STIs:
Specific antibiotics or antivirals, depending on the infection. - Prostatitis:
Longer antibiotics (sometimes several weeks) and anti-inflammatory medications. - Bladder or Kidney Stones:
May require painkillers, fluids to help pass the stone, or sometimes procedures to remove it. - Non-Infectious Irritation:
Avoid triggers (scented products, tight clothes). Topical creams or simply time to heal.
Other Options
- Pain Relief:
Over-the-counter painkillers (like paracetamol or ibuprofen). Special urinary pain medicines (phenazopyridine) may help, but only short-term. - Increased Fluids:
Drink more water to flush out bacteria. - Good Hygiene Practices:
Wipe front to back, urinate after sex, avoid irritants.
If symptoms are severe or keep coming back, see your doctor. They might need to dig deeper for less common causes.
References:
- Painful Urination (Dysuria). Mayo Clinic. 2024. https://www.mayoclinic.org/symptoms/painful-urination/basics/definition/sym-20050774
- Dysuria: Evaluation and Differential Diagnosis in Adults. American Family Physician (AAFP), August 15, 2020. https://www.aafp.org/pubs/afp/issues/2020/0815/p194.html
- Urinary Tract Infection (UTI). National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), July 2023. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-infections-utis
