Shoulder pain. Nearly everyone has felt it at some point. Maybe it’s a sharp twinge when reaching overhead, or a dull ache that keeps you up at night. It’s incredibly common—studies show that up to one in four people will experience shoulder pain in their lifetime. Whether you’re a weekend athlete or someone who just spends too long hunched over a keyboard, the shoulder is surprisingly easy to upset. But why?
What Is Shoulder Pain?
Shoulder pain is any discomfort you feel in or around the shoulder joint. It can be mild and fleeting, or severe enough to make everyday tasks—like brushing your hair or lifting a mug—feel impossible. The pain might be felt at the front, back, side, or even deep inside the joint. Sometimes, it’s even “referred” pain, meaning the problem starts somewhere else but you feel it in your shoulder.
Did you know the shoulder is the most mobile joint in the body? That flexibility, though, comes with a price: less stability. And that’s why the shoulder is so prone to injury.
How Does Shoulder Pain Happen?
Think of the shoulder as a super-flexible crane made of bones, muscles, and tendons, all working together. The main parts are:
- The ball-and-socket joint (where the upper arm bone fits into the shoulder blade)
- Rotator cuff (a group of muscles and tendons that keep everything in place)
- Bursa (tiny fluid-filled sacs that cushion movement)
With all these moving pieces, it doesn’t take much to throw things out of balance. Sometimes it’s a one-off injury—a fall or a heavy lift. Other times, it’s slow wear-and-tear from repeated motions. Even sitting with poor posture can start a chain reaction, like dominoes falling until you feel that familiar ache.
What Causes Shoulder Pain?
Let’s break it down. Shoulder pain isn’t one single condition—it has many faces. Here are the most common causes:
- Rotator cuff problems (about 70% of cases): This includes tears, tendinitis (inflammation), or impingement (tendons getting pinched).
- Frozen shoulder (adhesive capsulitis): Stiffness and pain that slowly get worse, often after an injury or period of not moving the shoulder.
- Arthritis: Wear-and-tear in the joint, leading to pain and limited movement.
- Bursitis: When the bursa (those little fluid sacs) become inflamed, usually from overuse.
- Shoulder dislocation: The ball pops out of the socket, often from a fall or accident.
- Referred pain: Sometimes, issues in your neck, heart, or even gallbladder can send pain signals to your shoulder.
To put it simply: If the shoulder moves the wrong way, too much, or for too long—it can hurt. But most cases are due to overuse or injury, not something serious.
Risk Factors
Who’s most likely to develop shoulder pain? You might be surprised.
- Age: Over 40? You’re more likely to get rotator cuff injuries or frozen shoulder.
- Jobs and sports: Painters, athletes (especially in sports like tennis, swimming, baseball), or anyone doing repetitive overhead motions.
- Posture: Slouching at a desk or carrying heavy bags on one shoulder.
- Previous injuries: Old injuries make future problems more likely.
- Diabetes: Raises your risk for frozen shoulder.
In short, anyone can get shoulder pain, but some lifestyles and habits tip the odds against you.
Other Symptoms
Shoulder pain rarely travels alone. You might also notice:
- Stiffness or reduced range of motion (hard to lift your arm or reach behind your back)
- Clicking or popping sounds
- Swelling or tenderness
- Weakness in the shoulder or arm
When things get worse, the pain can become constant, disrupt your sleep, or make it impossible to move your arm at all. In severe cases—like a major tear or dislocation—you might notice visible deformity or be unable to move the shoulder entirely.
Tests to Identify the Cause
Doctors usually start with a detailed history and physical exam, moving your arm in different ways to pinpoint what’s wrong. If the cause isn’t clear, or if surgery is being considered, they might order:
- MRI scan: The gold standard for soft tissue injuries (like rotator cuff tears).
- X-ray: Great for spotting bone problems, like arthritis or fractures.
- Ultrasound: Useful for checking tendons in real-time movement.
Don’t worry—most tests are painless. You just have to hold still while the machine does its work.
Treatment for Shoulder Pain
Here’s the good news: most shoulder pain gets better without surgery.
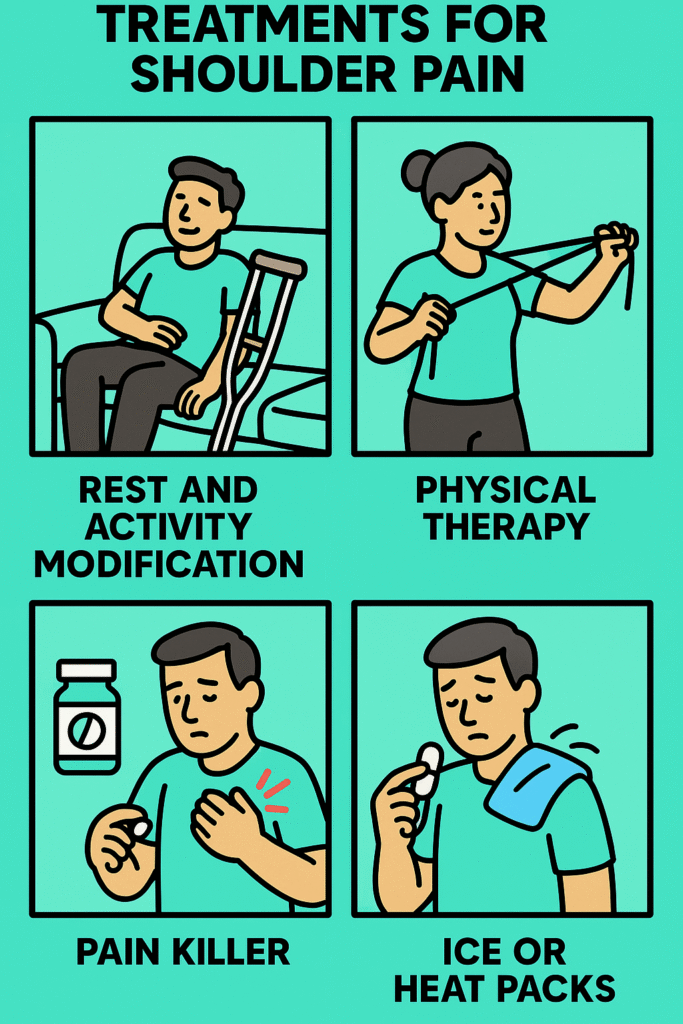
Mainstream (Gold Standard) Treatment
- Rest and activity modification: Let the shoulder heal; avoid heavy lifting or repetitive movements.
- Physical therapy: A tailored exercise plan is the backbone of recovery, restoring strength and flexibility.
- Pain relief: Over-the-counter medications like paracetamol or ibuprofen often help.
- Ice or heat packs: Reduce inflammation and ease stiffness.
Other Options
- Corticosteroid injections: For stubborn pain, especially if there’s lots of inflammation.
- Surgery: Reserved for severe injuries (like large rotator cuff tears or repeated dislocations), or if nothing else works after months of rehab.
- Alternative therapies: Acupuncture, massage, or chiropractic care—some people find them helpful, though evidence is mixed.
Above all, patience is key. Recovery can take weeks or months, but with the right plan, most people return to full function.
References
1. Shoulder Pain: Causes, Treatment, and When to See a Doctor. Mayo Clinic, 2024. https://www.mayoclinic.org/diseases-conditions/shoulder-pain/symptoms-causes/syc-20369060
2. Shoulder pain: Causes, diagnosis, and treatment. Harvard Health Publishing, 2023. https://www.health.harvard.edu/pain/shoulder-pain-causes-diagnosis-and-treatment
3. Shoulder pain. National Health Service (NHS), UK, 2023. https://www.nhs.uk/conditions/shoulder-pain/
