What is a Urinary Tract Infection?
Ever felt a burning sensation when you pee? Or that urgent, gotta-go feeling—only to produce a few drops? That could be a urinary tract infection, commonly known as a UTI.
A UTI is an infection in any part of your urinary system—kidneys, bladder, ureters, or urethra. Most infections involve the lower urinary tract, particularly the bladder and urethra. UTIs are extremely common, especially in women. In fact, about 50–60% of women will experience at least one UTI in their lifetime, while it’s less frequent in men【1】.
How does it occur?
Think of your urinary system as a highway for waste to exit the body. Normally, urine flows from the kidneys, down the ureters, into the bladder, and out through the urethra—flushing out bacteria along the way. But when bacteria (usually E. coli from the bowel) sneak into the urethra and multiply, they can cause inflammation and infection.
Imagine your bladder like a water balloon with an alarm system. When bacteria set up camp there, your body responds with inflammation—swelling, irritation, and pain—triggering that urgency to urinate even when the bladder isn’t full.
If left untreated, the infection can travel upwards to the kidneys—a serious condition known as pyelonephritis.
What are the causes of UTI?
UTIs are usually caused by bacteria, but not all bacteria are created equal. Let’s look at the main culprits:
- Escherichia coli (E. coli): This bacteria, which normally lives in the intestines, is behind 80–90% of UTIs【2】.
- Staphylococcus saprophyticus: A less common but notable cause, responsible for about 5–15% of UTIs, especially in younger women.
- Other bacteria: Such as Klebsiella, Proteus, and Enterococcus species.
- Fungal UTIs (rare): More likely to occur in people with weak immune systems.
Sometimes, UTIs also result from viruses or as complications from urinary catheters or surgeries.
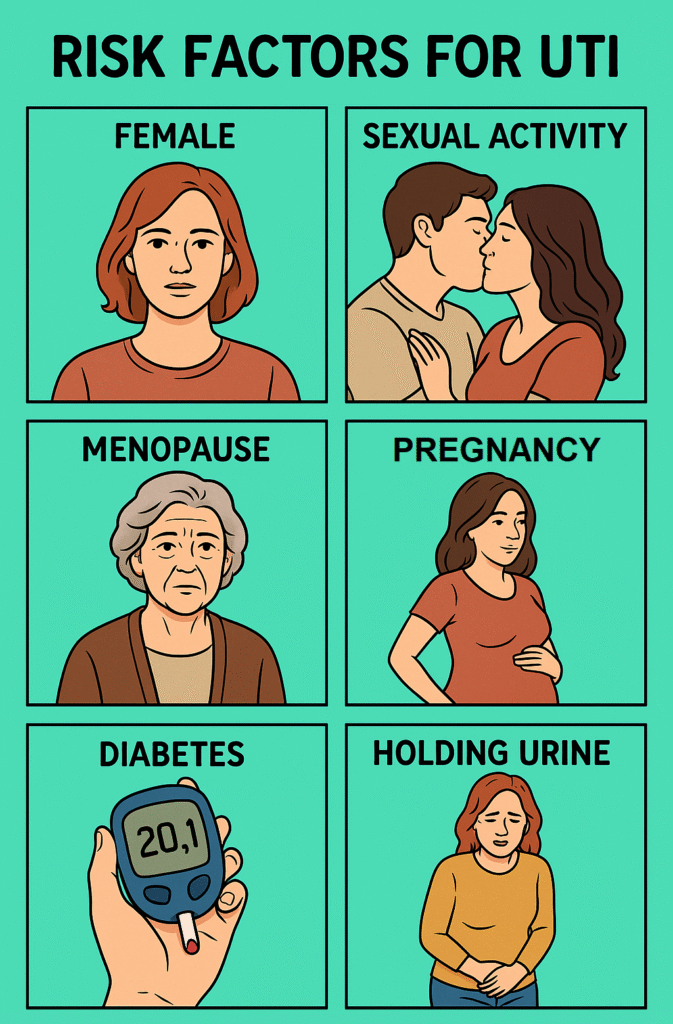
What are the risk factors?
UTIs don’t strike randomly. Certain situations make you more likely to get one.
Some of the top risk factors include:
- Being female: Shorter urethras mean bacteria reach the bladder more easily.
- Sexual activity: Bacteria can be pushed into the urethra during sex.
- Menopause: Lower estrogen levels reduce the protective vaginal flora.
- Pregnancy: Hormonal changes and pressure on the bladder increase UTI risk.
- Urinary catheters: These can introduce bacteria into the bladder.
- Diabetes: High sugar levels support bacterial growth.
- Holding in urine: Delaying urination gives bacteria more time to multiply.
Symptoms of UTI
So what does a UTI feel like?
You’ll know something’s off. The classic symptoms include:
- Burning sensation during urination: The hallmark sign.
- Frequent urination: That never-ending urge.
- Cloudy or strong-smelling urine
- Lower abdominal pain or pelvic pressure
- Blood in the urine (called hematuria)
- Feeling tired or shaky
- Fever and back pain (in more serious kidney infections)
Why do these symptoms occur? Because the bladder lining becomes inflamed—it’s like having a raw, irritated patch inside, and every drop of urine rubbing against it causes pain.
Differential Diagnosis
Many other conditions mimic UTI symptoms. It’s crucial not to jump to conclusions.
Here are some of the main differentials:
- Vaginitis (yeast or bacterial): Causes burning and discharge, often confused with UTIs.
- Interstitial cystitis: A chronic condition with UTI-like pain but no infection.
- Sexually transmitted infections (STIs): Like chlamydia or gonorrhoea.
- Urethritis: Inflammation of the urethra due to infection or irritation.
- Bladder stones or tumours: These can cause blood and pain during urination.
Proper testing helps tell them apart.
How is a UTI diagnosed?
Diagnosis is more than just guessing from symptoms. The gold standard is a urine microscopic examination or urine culture—a lab test that identifies the exact bacteria.
Here’s how it’s done:
- Clean-catch urine sample: You’ll be asked to clean the genital area and catch midstream urine in a sterile cup.
- Urinalysis: The sample is first tested for signs of infection (like white blood cells, nitrites).
- Urine culture: If needed, it’s sent to a lab to see what bacteria grow and which antibiotics work best.
In more serious or recurrent cases, imaging like ultrasound or CT scan may be needed to rule out kidney involvement or anatomical problems.
Treatment of UTI
Thankfully, most UTIs are easy to treat.
The first-line treatment? Antibiotics. But the exact choice depends on your health history and the bacteria involved.
Common antibiotics include:
- Nitrofurantoin (Macrobid)
- Trimethoprim-sulfamethoxazole (Bactrim)
- Fosfomycin (Monurol)
- Amoxicillin-clavulanate
- Ciprofloxacin (used more cautiously due to resistance issues)
You might feel better in a day or two, but always finish the full course to prevent recurrence.
For recurrent UTIs, doctors may recommend:
- Low-dose daily antibiotics for a few months
- Post-coital antibiotics (if UTIs are sex-related)
- Topical estrogen for postmenopausal women
Also, don’t underestimate non-antibiotic measures:
- Drink plenty of water
- Urinate frequently (don’t hold it!)
- Wipe front to back after using the toilet
- Avoid douches and scented feminine products
Final Thoughts
UTIs are common, painful, and sometimes scary—but they’re treatable and preventable. If you’re dealing with frequent infections, don’t suffer in silence. Talk to your doctor, ask questions, and get the right tests.
Your body is trying to tell you something. Listen to it.
References
- Medina, M., & Castillo-Pino, E. (2019). An introduction to the epidemiology and burden of urinary tract infections. Therapeutic Advances in Urology, 11, 1756287219832172. https://journals.sagepub.com/doi/10.1177/1756287219832172
- Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269–284. https://www.nature.com/articles/nrmicro3432
- Gupta, K., Hooton, T. M., & Naber, K. G. (2011). International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women. Clinical Infectious Diseases, 52(5), e103–e120. https://academic.oup.com/cid/article/52/5/e103/327289
