Summary
- Autoimmune thyroiditis is an immune-mediated disorder that leads to thyroid inflammation and dysfunction.
- Common symptoms include fatigue, weight changes, and sensitivity to cold or heat.
- Treatment focuses on hormone replacement therapy and monitoring thyroid hormone levels to manage symptoms.
Introduction
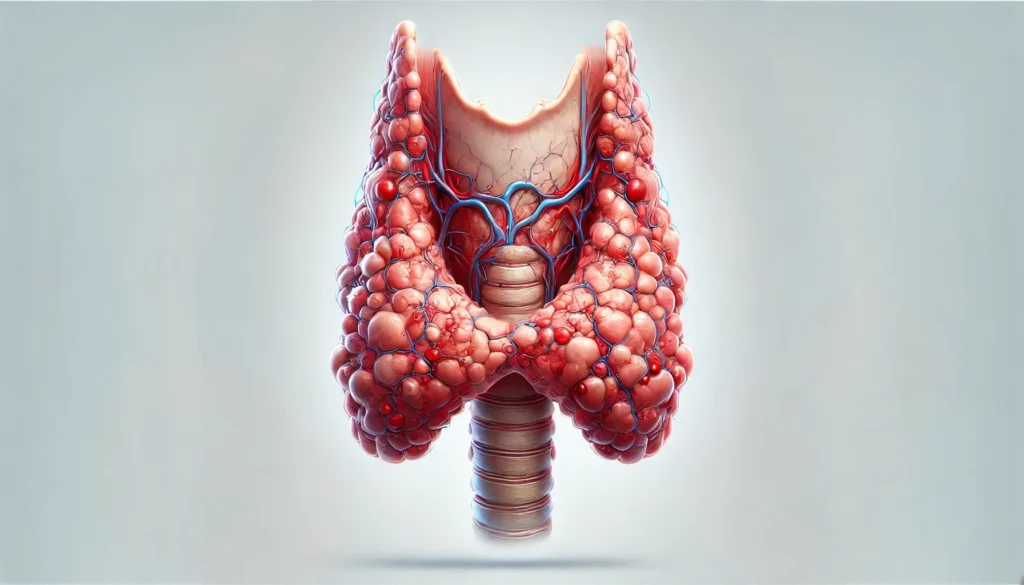
Autoimmune thyroiditis, called Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis, is the main cause of hypothyroidism (low thyroid function) in adults, mostly affecting women.
This condition happens when the immune system wrongly attacks the thyroid gland, causing long-term inflammation, reduced thyroid function, and, in the end, a shortage of thyroid hormones.
The thyroid gland makes hormones essential for managing metabolism, energy levels, and various body activities. Damage from autoimmune actions may slow these processes, resulting in several symptoms.
Autoimmune thyroiditis is a long-term issue that usually worsens gradually. The precise reason for the immune attack on the thyroid is not fully known, but genetic, environmental, and hormonal factors likely play crucial roles in its onset.
Causes
The exact reasons for autoimmune thyroiditis aren’t fully known, but several elements contribute to it:
1. Genetic Factors:
A family background of thyroid issues or autoimmune ailments raises the chances of getting autoimmune thyroiditis. Certain genes related to immune function are often present in those with the condition.
2. Immune System Issues:
Autoimmune thyroiditis happens when the body’s immune system targets its own thyroid cells.
The immune system makes antibodies against thyroid proteins, like thyroid peroxidase (TPO) and thyroglobulin (Tg).
These antibodies cause inflammation and harm the thyroid gland, affecting its hormone production.
3. Environmental Factors:
Some environmental triggers can elevate the risk of autoimmune thyroiditis, such as:
- Infections: Viral or bacterial infections can activate the immune system, possibly starting an autoimmune response.
- Iodine Levels: Both too much and too little iodine can affect thyroid function and may initiate autoimmune thyroiditis in those who are genetically inclined.
- Radiation: Childhood exposure to radiation connects to a higher risk of developing autoimmune thyroid diseases.
- Stress: Both physical and emotional stress might disturb immune regulation, which could lead to or worsen autoimmune thyroiditis.
4. Hormonal Factors:
The higher occurrence of the condition in women indicates that sex hormones might influence its development.
Pregnancy and menopause are critical times when the condition is likelier to show up, especially for those with a family history of autoimmune thyroid disease.
Symptoms
The signs of autoimmune thyroiditis appear slowly and may be mild initially.
The thyroid gland may first enlarge (known as a goiter) but could shrink later as damage increases.
The symptoms align with hypothyroidism because the gland cannot produce enough thyroid hormones. Typical symptoms include:
- Fatigue: A common hypothyroidism symptom, fatigue arises from slowed metabolic functions.
- Weight Gain: A slow metabolism can cause unwanted weight gain, even if eating habits do not change.
- Cold Sensitivity: Those with autoimmune thyroiditis often feel cold because of a slowed metabolism and decreased heat production.
- Dry Skin and Hair: Dryness and thinning of skin, hair, and nails are seen in those with the condition. Individuals with hypothyroidism may experience issues due to less blood flow and a decrease in skin cell renewal.
- Constipation: Slower movement in the digestive system can result in ongoing constipation.
- Depression: Mood changes and mental health problems, including depression, are common because a drop in thyroid hormones influences brain chemistry.
- Memory and Focus Problems: Cognitive abilities might weaken, leading to memory problems and difficulty focusing, often called “brain fog.”
- Muscle and Joint Discomfort: Weakness in muscles, stiffness, and joint pain may happen from hypothyroidism.
- Hoarseness and Swelling: The thyroid gland might enlarge (goiter), leading to hoarseness, neck swelling, or swallowing difficulties.
- Menstrual Irregularities: Women with autoimmune thyroiditis might face heavy or erratic menstrual cycles due to hormonal changes.
- Higher Cholesterol Levels: Higher cholesterol levels may arise from a slower metabolism.
The extent and variety of symptoms can differ based on the level of thyroid dysfunction and the person’s overall health.
Risk Factors
Several elements can raise the chances of developing autoimmune thyroiditis:
- Gender: Women are much more likely to develop autoimmune thyroiditis than men, with a ratio of about 7:1.
- Age: Autoimmune thyroiditis often affects adults, mainly those aged 30 to 50.
- Family History: A background of autoimmune diseases or thyroid issues, especially Hashimoto’s thyroiditis, heightens the risk of this condition.
- Other Autoimmune Conditions: Having a personal or family history of other autoimmune disorders, such as rheumatoid arthritis, lupus, or type 1 diabetes, raises the risk of autoimmune thyroiditis.
- Pregnancy: Pregnancy, especially postpartum, can instigate or intensify autoimmune thyroiditis due to immune system changes and hormonal shifts.
- Environmental Factors: Excess or lack of iodine, stress, infections, and contact with environmental toxins may increase the likelihood of developing autoimmune thyroiditis in predisposed individuals.
- Radiation Exposure: Childhood exposure to radiation is linked to a higher risk of autoimmune thyroid diseases, including Hashimoto’s thyroiditis.
Differential Diagnosis
Several other conditions have symptoms that resemble autoimmune thyroiditis, making it essential to exclude other potential causes of hypothyroidism and thyroid issues.
These conditions include:
- Subacute Thyroiditis: This is thyroid inflammation due to virus infections, usually accompanied by fever and neck pain. In contrast to autoimmune thyroiditis, subacute thyroiditis generally resolves on its own, and thyroid function typically normalizes after a few months.
- Hypothyroidism from Iodine Deficiency: Lack of iodine can cause hypothyroidism, which may lead to symptoms like those seen in autoimmune thyroiditis. However, iodine deficiency usually brings about a goiter (enlarged thyroid) and can be addressed with iodine supplements.
- Thyroid Cancer: Though uncommon, thyroid cancer can show as a goiter and have symptoms similar to autoimmune thyroiditis. Fine needle aspiration (FNA) or biopsy may be needed to distinguish between the two.
- Pituitary or Hypothalamic Disorders: Secondary hypothyroidism from issues in the pituitary or hypothalamus can cause low thyroid hormone levels. However, the reasons for secondary hypothyroidism differ from those of autoimmune thyroiditis.
- Drug-Induced Hypothyroidism: Some medications, like lithium or amiodarone, can affect thyroid function and simulate the symptoms of autoimmune thyroiditis.
- Graves’ Disease: Graves’ disease is another autoimmune thyroid condition. Disorder, unlike Hashimoto’s thyroiditis, causes hyperthyroidism (too much thyroid activity) instead of hypothyroidism (too little). To tell Graves’ disease apart from Hashimoto’s thyroiditis, look for a goiter, thyroid antibodies, and signs of hyperthyroidism.
| Differential Diagnosis | Definition | Symptoms | Treatment |
|---|---|---|---|
| Autoimmune Thyroiditis | Chronic autoimmune inflammation of the thyroid leading to hypothyroidism. | Fatigue, weight gain, cold intolerance, and goiter. | Thyroid hormone replacement therapy (levothyroxine). |
| Subacute Thyroiditis | Thyroid inflammation caused by viral infections, typically self-limiting. | Fever, neck pain, and temporary thyroid dysfunction. | Supportive care with NSAIDs or corticosteroids for pain and inflammation. |
| Hypothyroidism from Iodine Deficiency | Low thyroid hormone production due to insufficient iodine intake. | Goiter, fatigue, and symptoms of hypothyroidism. | Iodine supplementation or dietary changes to increase iodine intake. |
| Thyroid Cancer | Malignant growth in the thyroid gland. | Neck lump, hoarseness, and difficulty swallowing. | Surgical removal of the thyroid gland, radioactive iodine therapy, or chemotherapy. |
| Pituitary or Hypothalamic Disorders | Secondary hypothyroidism caused by dysfunction in the pituitary or hypothalamus. | Fatigue, cold intolerance, and low thyroid hormone levels. | Treatment of the underlying pituitary or hypothalamic condition. |
| Drug-Induced Hypothyroidism | Thyroid dysfunction caused by medications such as lithium or amiodarone. | Symptoms similar to hypothyroidism, including fatigue and weight gain. | Discontinuation of the offending drug or thyroid hormone replacement if needed. |
| Graves’ Disease | An autoimmune disorder causing hyperthyroidism. | Weight loss, heat intolerance, tremors, and goiter. | Antithyroid medications, radioactive iodine therapy, or thyroidectomy. |
Investigation
To diagnose autoimmune thyroiditis and check thyroid issues, a mix of clinical tests, lab tests, and imaging is needed:
1. Blood Tests:
Thyroid Function Tests: Testing serum thyroid hormones, like thyroxine (T4) and triiodothyronine (T3), with thyroid-stimulating hormone (TSH) is important to find hypothyroidism. In autoimmune thyroiditis, TSH is high, while T4 and T3 are low.
Thyroid Antibodies: Finding specific thyroid antibodies, like anti-thyroid peroxidase (TPO) and anti-thyroglobulin (Tg), shows autoimmune thyroiditis. High levels of these antibodies show an autoimmune reaction against the thyroid.
Anti-TSH Receptor Antibodies: These are checked if other thyroid problems, like Graves’ disease, are suspected.
Ultrasound: A thyroid ultrasound looks at the size and shape of the thyroid, finds nodules, or checks for a goiter. In autoimmune thyroiditis, the gland may seem uneven or enlarged.
Fine Needle Aspiration (FNA): If any nodules look suspicious, FNA may be done to exclude thyroid cancer or other issues.
2. Imaging:
A thyroid ultrasound can check for any enlargement, nodules, or unevenness.
It’s not always needed for diagnosis but can provide useful details in some cases.
Treatment
Treating autoimmune thyroiditis mainly aims to manage hypothyroidism and symptoms. Key strategies include:
1. Thyroid Hormone Replacement Therapy:
The main treatment involves synthetic thyroid hormones, usually levothyroxine (T4), to adjust thyroid levels. The dose varies based on blood results, age, weight, and hypothyroidism intensity.
The aim is to restore normal thyroid hormone levels and reduce hypothyroid symptoms like fatigue, weight gain, and feeling cold.
This treatment usually lasts a lifetime, and patients need regular follow-up for thyroid function tests to confirm the correct dosage.
2. Monitoring:
Regular checks of thyroid function are crucial to get the right levothyroxine dose.
Normally, TSH and free T4 blood tests are done every 6-12 weeks after starting. Once the proper dose is found, testing can switch to yearly.
Monitoring is also vital during pregnancy, as thyroid hormone needs can shift, needing dose adjustments.
3. Management of Goiter:
Sometimes, the thyroid might stay enlarged (goiter) even with treatment. If the goiter causes issues like swallowing or breathing problems, more treatment might be needed, which can include:
- Surgical Intervention: In rare instances, if the goiter leads to serious symptoms or is thought to be cancerous, surgery (thyroidectomy) might be necessary.
- Radioactive Iodine: Though not generally used for autoimmune thyroiditis, radioactive iodine can help shrink the thyroid gland in cases of hyperthyroidism, such as Graves’ disease if it develops later.
4. Symptomatic Treatment:
People with autoimmune thyroiditis often face issues like depression, weight gain, and fatigue. Management can include lifestyle changes, such as more exercise, good nutrition, and stress-reduction techniques.
Medications like antidepressants may also be prescribed for mood issues.
5. Managing Other Health Issues:
Many people with autoimmune thyroiditis also have other autoimmune problems, like type 1 diabetes, rheumatoid arthritis, or vitiligo. It is important to manage these alongside thyroid treatment for better overall health.
6. Considerations During Pregnancy:
Women with autoimmune thyroiditis who are pregnant need careful monitoring of their thyroid levels.
If hypothyroidism is not controlled during pregnancy, risks such as miscarriage, premature birth, and developmental problems for the baby can increase.
Pregnant women may need changes to their levothyroxine dosage, as the need for thyroid hormones rises during pregnancy.
Prognosis
The outlook for those with autoimmune thyroiditis is usually good with proper treatment. Most individuals can live normal lives after starting thyroid hormone replacement therapy and keeping thyroid levels normal.
However, not treating hypothyroidism can lead to issues like heart disease, infertility, mental health problems, and in severe cases, myxedema coma, which is very serious.
Conclusion
Autoimmune thyroiditis, known as Hashimoto’s thyroiditis, is a common reason for hypothyroidism that needs continuous management.
Though the specific cause is not completely clear, both genetic and environmental factors are important in its occurrence. Early detection and proper treatment, especially with thyroid hormone replacement therapy, allow those with autoimmune thyroiditis to live healthy, normal lives.
Ongoing monitoring, managing symptoms, and making lifestyle changes are key for the best health results. While autoimmune thyroiditis is generally not life-threatening, untreated or poorly managed hypothyroidism can lead to serious health problems.
- Cooper, D. S., & Biondi, B. (2012). “Subclinical thyroid disease.” The Lancet, 379(9821), 1142-1154.
- Weetman, A. P. (2000). “Autoimmune thyroid disease.” Autoimmunity Reviews, 1(4), 101-107.
- Wartofsky, L., & Dickey, R. A. (2005). “The thyroid and its diseases.” The Journal of Clinical Endocrinology & Metabolism, 90(3), 1256-1262.
- Ross, D. S., & Burch, H. B. (2016). “Management of Hashimoto’s thyroiditis.” Thyroid Disease Manager. Available at: https://www.thyroidmanager.org
- American Thyroid Association. (2020). “Hashimoto’s Thyroiditis: An Overview.” Available at: https://www.thyroid.org/hashimotos-disease